Who is a Medical Doctor?
What Doctors can do or don't do?
Doctors have medical training. Doctors often specialise.
Doctors do diagnose illness and prescribe treatments.
Doctors claim to use science based methods.
Doctors are not trained in dietary nutrition.
Doctors are not responsible for public health.
A Very Brief History of Medical Training
Over 100 years ago, there was serious competition between "doctors" who sold "Natural Cures" by the bottle or the pill, usually just traveling salesmen, with a pitch about "Dr Mason's Liver Pills" or something similar, and medical doctors, who had some formal medical training. The best were probably trained in Europe, in Austria or Germany, at some established medical institute.
The first formal training of medical doctors in the USA began in 1765. Many new "medical schools" opened but the standards were poor. Medical training in Europe was much more advanced. In the 1870's, The American Medical Association was established. The AMA published in 1906 the first American Medical Directory, which list 128,000 licensed physicians in the U.S. and Canada. The American Medical Association was concerned about the variability of professional standards. (Who should be listed in the American Medical Directory was hotly disputed. Who is, or is not, a medical doctor?)
In 1908, the Council on Medical Education contracted with the Carnegie Foundation for the Advancement of Teaching to survey American medical education. Abraham Flexner was employed to writing this report, Flexner visited every one of the one hundred fifty-five North American medical schools then in operation, and wrote a damming report. He described Chicago's fourteen medical schools, for example, as "a disgrace to the State whose laws permit its existence . . . indescribably foul . . . the plague spot of the nation." Flexner found John Hopkins School of Medicine, to be a "small but ideal medical school, embodying ... the best features of medical education in England, France, and Germany." (Within a few years the number of "medical schools" reduced by more than 50%.)
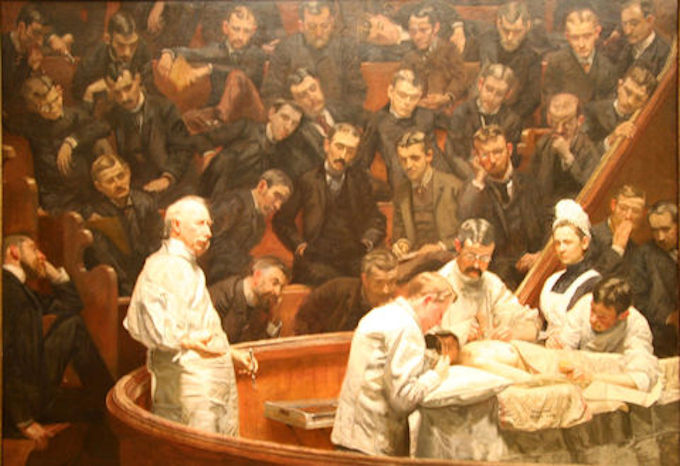
Surgical Training, USA, 1889
Even in 1910, the regulation of the medical profession in the USA, by state governments was minimal or nonexistent. American doctors varied enormously in their scientific understanding of human physiology, and the word "quack" flourished. In the USA, as late as the 1930's medical doctors were still striving to establish themselves as true medical professionals.
That is why doctors are not trained in nutrition. To recommend dietary change is not offering a medical cure. That's what a non-professional would recommend. Doctor's offer "scientifically proven" medical solutions for health problems. Distancing between real doctors and quacks, was a strategically important issue.
[From Wikipedia] "Medical schools that offered training in various disciplines including electromagnetic field therapy, phototherapy, eclectic medicine, physiomedicalism, naturopathy, and homeopathy, were told either to drop these courses from their curriculum or lose their accreditation." Doctors henceforth are required to use scientific methods of diagnosis and treatment. But progress has been slow, most often current practice was called "scientific" even when it clearly wasn't so.
 Excellent evidence of that was the largest scientific study ever done of "modern" medical and health advice, based on medical practice and protocols in the 1980's.
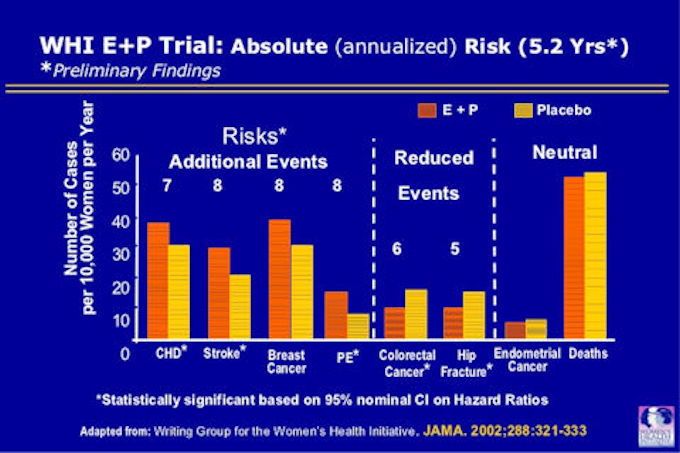
Excellent evidence of that was the largest scientific study ever done of "modern" medical and health advice, based on medical practice and protocols in the 1980's. ![]() The Woman's Health Initiative. The main studies were the hormone trial and the dietary trial. The results of the study were shocking. All of the main objectives of the study failed. To the researchers credit, when it became clear that for some people the recommended protocol was causing early deaths, they stopped the research (1998). For several years they tried to make the evidence fit what they expected to find. They felt that couldn't publish the results, that disproved all of their prior hypotheses.
The Woman's Health Initiative. The main studies were the hormone trial and the dietary trial. The results of the study were shocking. All of the main objectives of the study failed. To the researchers credit, when it became clear that for some people the recommended protocol was causing early deaths, they stopped the research (1998). For several years they tried to make the evidence fit what they expected to find. They felt that couldn't publish the results, that disproved all of their prior hypotheses.
When they did finally publish (2006), they swept the failures under the carpet. Dr Paul Mason says; "Only one significant finding (of the WHI) - not mentioned in conclusion or results section - was buried in obscure text on page 661 of the journal. A low fat diet increased cardiac events by 26% in females with pre-existing heart issues."
What happened next? Nothing; silence; you need to search for any mention of the Women's Health Initiative, There was too much money, prestige, and future income that depended on in current training and medical practice. In NIH laboratories, hospital procedures and university programs, too much money was committed for years ahead, to suddenly stop because of new scientific evidence. ![]() Dr Elizabeth Nabel on behalf the NIH seemed to be saying, "We want medicine to be guided by science, but not yet please." Her actual statement laid emphasis on the continued need to reduce the saturated fat in the diet. The WHI, had now proven that contrary to advice given by experts for at least 50 years, that restricting saturated fats was at least an unhelpful practice. In some women eating a low saturated fat diet increased adverse cardiac events by 20%.
Dr Elizabeth Nabel on behalf the NIH seemed to be saying, "We want medicine to be guided by science, but not yet please." Her actual statement laid emphasis on the continued need to reduce the saturated fat in the diet. The WHI, had now proven that contrary to advice given by experts for at least 50 years, that restricting saturated fats was at least an unhelpful practice. In some women eating a low saturated fat diet increased adverse cardiac events by 20%.
Even so, four years later, the 2010 Dietary Guidelines did not change the recommendation of the past 30 years. They ignored the WHI finding. The Dietary Guidelines for 2015 quietly dropped the adverse recommendation to avoid saturated fat. The Dietary Guidelines 2020, still haven't accepted that the WHI has demonstrated that the Dietary Guidelines themselves are wrong. Very powerful forces are preventing change. We are not yet scientific, because some of our experts choose not to read, or refuse to accept, some of the current evidence.
From Wikipedia: The term "evidence-based medicine" was introduced in .... the autumn of 1990, by Gordon Guyatt, who used it in an unpublished description of a program at McMaster University for prospective or new medical students. Between 1993 and 2000, the Evidence-based Medicine Working Group at McMaster University published the methods to a broad physician audience in a series of 25 "Users' Guides to the Medical Literature" in JAMA. In 1995 Rosenberg and Donald defined individual level evidence-based medicine as "the process of finding, appraising, and using contemporaneous research findings as the basis for medical decisions."
So today we are trained to think that a doctor will diagnose a disease and recommend a cure. One problem should have one remedy. We are looking to a doctor for a medical solution, guaranteed to work. The medical profession tried hard to separate the professional doctor from quacks. Since "natural cures" were often based on the idea that some foods were super-foods, and might resolve health problems, doctors are reluctant to suggest food as a solution to health problems.
The unfortunate legacy of this is our inability to resolve many chronic "diseases" that are caused by diet or lifestyle, by medical methods. Examples are many auto-immune diseases, obesity, tooth decay, type II diabetes, maybe Alzheimer's and several gut and bowel problems.
Are we looking in the wrong direction for a solution? Obesity, tooth decay, type II diabetes, are at the essence NOT medical problems, they are failures of the public health system. Just as a good public health system can stop 23 million people getting Covid-19 as Taiwan has demonstrated, it should also be able to stop people from becoming obese.
![]() Open Future Health has a website that speaks to these issues. Dr Paul Mason, from Sydney, Australia, has been applying this knowledge in treating metabolic syndrome and arthritis. His patients have achieved dramatic and sustained weight loss and reductions in joint pain. Dr. Mason has recently become the Chief Medical Officer of Defeat Diabetes.
Open Future Health has a website that speaks to these issues. Dr Paul Mason, from Sydney, Australia, has been applying this knowledge in treating metabolic syndrome and arthritis. His patients have achieved dramatic and sustained weight loss and reductions in joint pain. Dr. Mason has recently become the Chief Medical Officer of Defeat Diabetes.
Defeat Diabetes is Australia's first evidence-based and doctor-led program that focuses on the wide range of health benefits of a low carb lifestyle, particularly for those wanting to send into remission pre-diabetes, type 2 diabetes, and other metabolic illnesses.
I this video, Dr. Mason delivers ![]()
![]() an hour long lecture explaining the current science for trainee medical doctors.
an hour long lecture explaining the current science for trainee medical doctors.
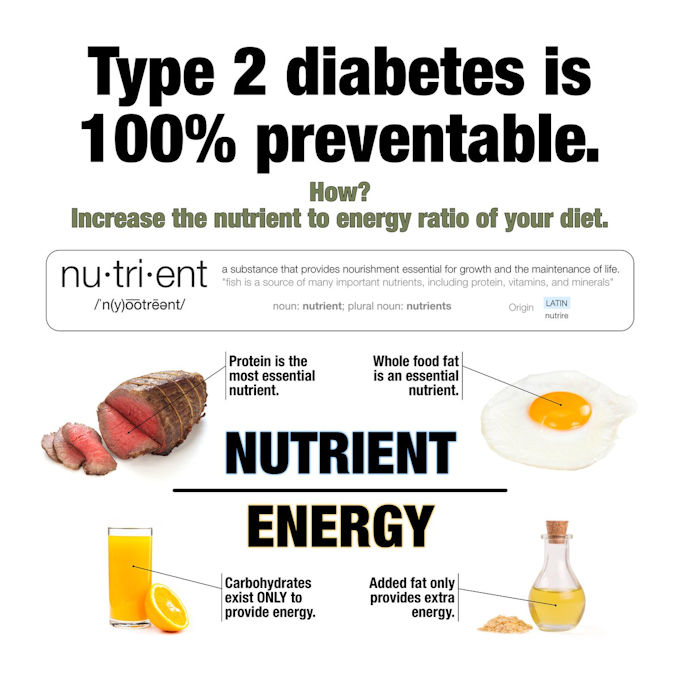
Type II Diabetes is not caused by obesity, but like obesity it is caused by lifestyle and diet, so it's 100% preventable, and a good public health system should have that objective. Calling on the doctor to "cure" diabetes after the system has failed is the ambulance at the bottom of the cliff. Where is the preventive fence at the top of the cliff?
Are you a doctor or do you know a doctor? Are you interested in low carb? Then this great new free course – low carb for doctors – could be something for you to watch or share!
This is the first part, featuring Dr. David Unwin, a family physician in England, who's involved in educating doctors and has been treating patients with low carb diets since 2012.
Dietitians become Professionals
One can argue the dietitians are a specialist profession, that should offer dietary advice. Sadly, dietitians are trapped by history too. Until the 1930's the text books used to train dietitians were written by members of the Seventh Day Adventist Church. The Church promotes vegetarian diets.
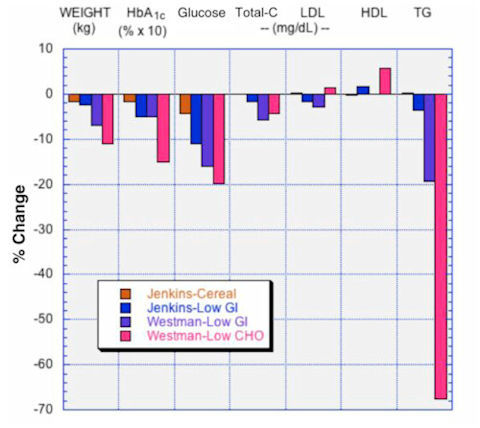
Above, four diets are compared. High carbohydrate, two versions of a low glycemic index diet, and a low carbohydrate diet. It's easy to see which diet produces the best metabolic outcome.
Even today, many dietitians imagine that the Mediterranean diet is the gold standard for human nutrition. They usually interpret the Mediterranean diet as vegetarian, or mostly vegetarian. The Mediterranean diet used for nutritional studies is mostly vegetarian, in contrast the actual diets eaten in the geographical region are quite different. (Mediterranean diet is different things for different purposes; to promote tourism, or to sell books, for instance.) Until recently, most dietitians were taught very little biochemistry.
In 2000, a dietitian, making a second career as a medical doctor asked Prof. Richard D Feinman, to incorporate some nutritional information as taught to dietitians into his biochemistry course. She supplied some texts from her prior training. Those texts, were full of biochemical errors and misunderstandings. Over the next few years Prof. Feinman developed a whole course on biochemistry and nutrition for dietitians, and medical trainees. Very few dietitians get this sort of training, even today. As with medicine, changing the capability of a profession takes a decade or more. In 2019 Dr Richard David Feinman, published a book, "![]() Nutrition in Crisis - Flawed Studies, Misleading Advice, and the Real Science of Human Metabolism."
Nutrition in Crisis - Flawed Studies, Misleading Advice, and the Real Science of Human Metabolism."
Public Health Professionals
"Public health professionals focus on preventing disease and injury by promoting healthy lifestyles. They implement educational programs, develop policies, administer services, conduct research, and regulate health systems to achieve these goals."
For most of us this is the most boring topic, the topic we don't want to read about. Covid-19 demonstrates how wrong that idea can be. We think that the long lives most people today expect to live is the result of medical advances. In fact it's the public health advances that have saved and extended the most lives. When Public Health operates well it's invisible. Only when there is a public health failure do we become concerned, and then we tend to look to medical options, instead of asking why did this happen at all?
Public Health successes have been in the control of pandemic infections, influenza, HIV-AIDS, SARS-CoV-1, and recently SARS-CoV-2. But public health is everywhere neglected, and success as demonstrated in Taiwan, has to be compared with failure as in Italy, and in the USA.
Public Health successes are in the field of medical drug regulation. The approval of drugs for specific uses, and the regulation of drug manufacture.
Public Health successes include accident prevention and safety in the work environment.
Public Health successes and sadly many failures involve the regulation and control of the production and disposal of waste products from manufacturing processes.
Public health failure is very obvious in the "war on drugs" which has been a disaster world-wide.
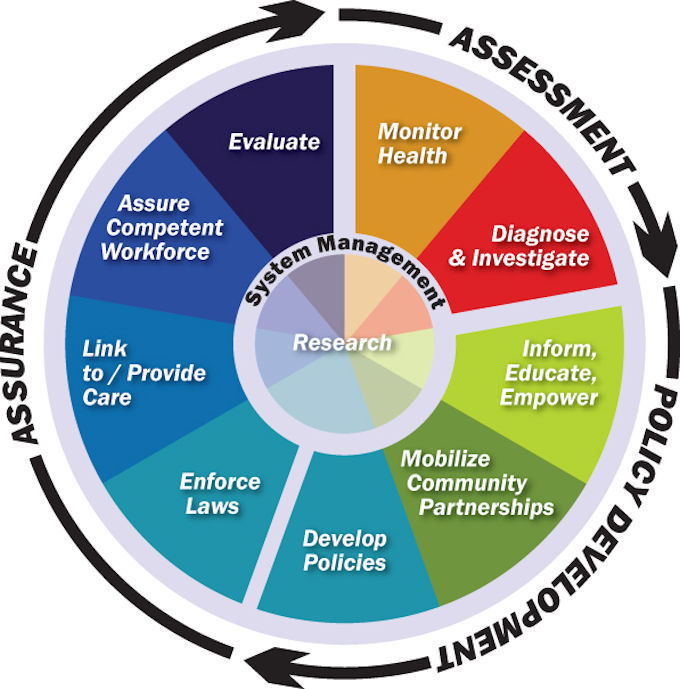
Public Health failure is most obvious in the fact that the major things that kill people are freely available on the open market. Vice Admiral C. Everett Koop, US Navy's chief medical officer, was appointed USA Surgeon General, by President Ronald Reagan. In his new role, Koop became concerned about the causes of modern diseases. He said that; "People buy the things that make them ill and cause their early death." That made him very unpopular with his political masters, and with industry. Perhaps also with many of the public. Koop was accused of wanting a "Nanny State." Koop served from 1982 to 1989, resisting pressure to change his views.
That highlights a critical issue. As Dr Koop said, we know that people buy the things that cause diseases that kill them. Should people be "free" to do that, or is some regulation of the market, possible and necessary? We have seen this issue clearly with the sale of tobacco, and alcohol. Our thinking about the sale of soft drinks, bread, red meat, lollies, marijuana, hand-guns and many other products is confused.
I occasionally do some market research. A smoker I spoke to said; "I've been smoking since I was 14 years old. I know that this product is killing me (Showing me what he just purchased.) but I'm addicted to nicotine, and dying early is the extra price I pay, over and above the $32.00 I just spent." So I ask you, who's to blame?
Stand outside a supermarket, in the 90 minutes before school starts, any morning. Breakfast; a block of chocolate, a bag of potato chips and a large soft drink. How many of these children are obese? Far too many of them. Why is this happening, because 50 years ago it didn't happen at all? Who is to blame for the tooth decay, the obesity, the fatty liver disease and the type II diabetes these children have? What can public health do about it?